If Your Uterus Ruptures Can You Have More Babies
| Uterine rupture | |
|---|---|
| Specialty | Obstetrics |
| Symptoms | Increased pain, vaginal bleeding, change in contractions[i] [two] |
| Usual onset | During labor[three] |
| Take a chance factors | Vaginal nascence after cesarean department, other uterine scars, obstructed labor, induction of labor, trauma, cocaine use[one] [4] |
| Diagnostic method | Supported by a rapid driblet in the infant's heart rate[i] |
| Handling | Surgery[i] |
| Prognosis | 6% adventure of babe decease[1] |
| Frequency | 1 in 12,000 vaginal deliveries with a normal uterus[ane] 1 in 280 with vaginal nativity afterwards cesarean section[1] |
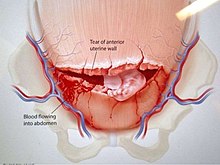
Transeverse uterine rupture
Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth.[3] Symptoms, while classically including increased hurting, vaginal bleeding, or a change in contractions, are not always present.[ane] [ii] Inability or decease of the mother or baby may consequence.[1] [3]
Risk factors include vaginal birth afterwards cesarean section (VBAC), other uterine scars, obstructed labor, induction of labor, trauma, and cocaine use.[1] [4] While typically rupture occurs during labor it may occasionally happen earlier in pregnancy.[three] [1] Diagnosis may be suspected based on a rapid drop in the baby'south heart charge per unit during labor.[1] [4] Uterine dehiscence is a less severe condition in which there is only incomplete separation of the former scar.[i]
Handling involves rapid surgery to control haemorrhage and commitment of the infant.[1] A hysterectomy may exist required to control the bleeding.[1] Blood transfusions may exist given to replace blood loss.[1] Women who have had a prior rupture are more often than not recommended to accept C-sections in subsequent pregnancies.[five]
Rates of uterine rupture during vaginal birth following one previous C-section, done by the typical technique, are estimated at 0.nine%.[one] Rates are greater among those who accept had multiple prior C-sections or an singular blazon of C-section.[ane] In those who do have uterine scarring, the risk during a vaginal nascency is near ane per 12,000.[1] Risk of death of the babe is about half-dozen%.[i] Those in the developing world announced to exist affected more often and have worse outcomes.[6] [3]
Signs and symptoms [edit]
Symptoms of a rupture may exist initially quite subtle. An old cesarean scar may undergo dehiscence; with further labor the woman may experience abdominal pain and vaginal haemorrhage, though these signs are hard to distinguish from normal labor. Oft a deterioration of the fetal heart rate is a leading sign, simply the cardinal sign of uterine rupture is loss of fetal station on manual vaginal examination. Intra-abdominal bleeding can lead to hypovolemic stupor and decease. Although the associated maternal mortality is at present less than one percent, the fetal mortality rate is between 2 and half-dozen percent when rupture occurs in the hospital.
In pregnancy uterine rupture may crusade a feasible intestinal pregnancy. This is what accounts for most abdominal pregnancy births.
- Intestinal hurting and tenderness. The pain may not be astringent; it may occur of a sudden at the peak of a contraction. The woman may describe a feeling that something "gave way" or "ripped."
- Chest hurting, pain between the scapulae, or pain on inspiration—Pain occurs because of the irritation of claret below the woman'due south diaphragm
- Hypovolemic shock acquired by bleeding, evidenced by falling claret pressure, tachycardia, tachypnea, pallor, cool and clammy skin, and anxiety. The fall in claret pressure is oftentimes a late sign of haemorrhage
- Signs associated with fetal oxygenation, such equally tardily deceleration, reduced variability, tachycardia, and bradycardia
- Absent fetal center sounds with a large disruption of the placenta; absent-minded fetal middle action by ultrasound examination
- Cessation of uterine contractions
- Palpation of the fetus outside the uterus (usually occurs only with a large, consummate rupture). The fetus is likely to exist expressionless at this point.
- Signs of an abdominal pregnancy
- Mail service-term pregnancy
Take chances factors [edit]
A uterine scar from a previous cesarean department is the almost common risk factor. (In ane review, 52% had previous cesarean scars.)[vii] Other forms of uterine surgery that result in total-thickness incisions (such equally a myomectomy), dysfunctional labor, labor augmentation by oxytocin or prostaglandins, and high parity may too set the phase for uterine rupture. In 2006, an extremely rare case of uterine rupture in a first pregnancy with no risk factors was reported.[8]
Uterine rupture during pregnancy without a prior cesarean section is 1 of the major diagnostic criterion for vascular Ehlers-Danlos syndrome (vEDS).[nine]
Mechanism [edit]
In an incomplete rupture the peritoneum is still intact. With a complete rupture the contents of the uterus spill into the peritoneal cavity or the broad ligament.
Treatment [edit]
Emergency exploratory laparotomy with cesarean delivery accompanied past fluid and blood transfusion are indicated for the management of uterine rupture. Depending on the nature of the rupture and the condition of the patient, the uterus may exist either repaired or removed (cesarean hysterectomy). Delay in management places both mother and kid at significant gamble.
See also [edit]
- Uterine perforation
References [edit]
- ^ a b c d e f g h i j k l m n o p q r s t Toppenberg, KS; Block WA, Jr (i September 2002). "Uterine rupture: what family physicians demand to know". American Family Doctor. 66 (v): 823–8. PMID 12322775.
- ^ a b Lang, CT; Landon, MB (March 2010). "Uterine rupture as a source of obstetrical hemorrhage". Clinical Obstetrics and Gynecology. 53 (one): 237–51. doi:10.1097/GRF.0b013e3181cc4538. PMID 20142660.
- ^ a b c d e Murphy, DJ (April 2006). "Uterine rupture". Electric current Stance in Obstetrics & Gynecology. 18 (2): 135–40. doi:10.1097/01.gco.0000192989.45589.57. PMID 16601473. S2CID 23617249.
- ^ a b c Mirza, FG; Gaddipati, Due south (April 2009). "Obstetric emergencies". Seminars in Perinatology. 33 (2): 97–103. doi:ten.1053/j.semperi.2009.01.003. PMID 19324238.
- ^ Larrea, NA; Metz, TD (January 2018). "Pregnancy Later Uterine Rupture". Obstetrics and Gynecology. 131 (1): 135–137. doi:ten.1097/AOG.0000000000002373. PMID 29215521.
- ^ Berhe, Y; Wall, LL (November 2014). "Uterine rupture in resource-poor countries". Obstetrical & Gynecological Survey. 69 (11): 695–707. doi:10.1097/OGX.0000000000000123. PMID 25409161. S2CID 22593593.
- ^ Chibber R, El-Saleh E, Fadhli RA, Jassar WA, Harmi JA (March 2010). "Uterine rupture and subsequent pregnancy consequence - how safe is it? A 25-year study". J Matern Fetal Neonatal Med. 23 (5): 421–iv. doi:ten.3109/14767050903440489. PMID 20230321. S2CID 13566623.
- ^ Walsh CA, O'Sullivan RJ, Foley ME (2006). "Unexplained prelabor uterine rupture in a term primigravida". Obstetrics and Gynecology. 108 (3 Pt 2): 725–7. doi:10.1097/01.AOG.0000195065.38149.11. PMID 17018479. S2CID 8021433.
- ^ Byers, Peter H. (2019). Vascular Ehlers-Danlos Syndrome. University of Washington, Seattle.
External links [edit]
Source: https://en.wikipedia.org/wiki/Uterine_rupture
0 Response to "If Your Uterus Ruptures Can You Have More Babies"
Postar um comentário